
The Real Life Difference Between Hospice and Palliative Care: Understanding Eligibility, Services, and Care Options
Hospice care and palliative care both enhance comfort and quality of life for people facing serious health challenges, yet they serve distinct roles in patient journeys. Recognizing when to begin each approach can relieve stress for patients, families, and caregivers while improving symptom management and emotional support. In this guide, you will learn:
- Core definitions and eligibility for hospice care.
- Palliative care’s timing, goals, and service scope.
- Direct comparisons of treatment focus, care settings, and payment options.
- Decision-making cues for selecting hospice versus palliative services.
- The interdisciplinary teams behind each model and their support offerings.
- Coverage details under Medicare, Medicaid, and private insurance.
- Common misconceptions clarified.
- Recent market trends, utilization data, and technology advances.
By mapping these themes, you’ll gain clarity on care pathways that best support your loved one’s needs and values.
What Is Hospice Care? Definition, Eligibility, and Focus on Terminal Illness
Hospice care is a specialized form of medical therapy designed for patients with a terminal illness and a prognosis of six months or less, when curative treatment is no longer pursued. It emphasizes comfort and holistic support rather than disease reversal. Typical hospice services enhance pain control, emotional well-being, and spiritual needs through an interdisciplinary team, improving overall quality of life in the final phase.
This approach connects directly to eligibility criteria, which hinge on prognosis and patient choice. Understanding these requirements provides context for comparing hospice care with broader palliative interventions.
How Is Hospice Care Defined and Who Is Eligible?

Hospice care is defined as comfort-oriented support for patients with a terminal medical condition and a life expectancy under six months as certified by two physicians. Eligibility requires that the patient forgo curative treatment, opting instead for symptom relief and family support. This ensures resources focus on pain management, psychosocial counseling, and end-of-life planning rather than aggressive therapies.
Clinicians confirm prognosis using disease trajectories—for example, advanced cancer staging or progressive organ failure—which lays groundwork for goal-of-care discussions and care planning.
What Are the Main Goals and Treatment Focus of Hospice Care?
Hospice care prioritizes pain control, symptom relief, and emotional support over attempts to cure the underlying disease. Its multidisciplinary team uses medication adjustments, complementary therapies, and counseling to enhance comfort. Spiritual care and bereavement services further support patients and families through loss and grief.
Focusing solely on comfort care ensures that interventions align with patient preferences, reducing hospitalizations and invasive procedures in the final months of life.
Which Conditions Qualify as Terminal Illness for Hospice?
Conditions commonly qualifying for hospice include advanced-stage cancers, end-stage heart failure, severe COPD with frequent exacerbations, late-stage dementia, and ALS. Prognostic criteria vary by disease but generally require evidence of steady decline despite optimal treatment. For instance, repeated hospital admissions for heart failure exacerbation signal eligibility.
Identifying qualifying illnesses clarifies when hospice care becomes the appropriate focus and prepares families for care transitions. This understanding leads naturally to exploring palliative care’s broader role in serious illness management.
What Is Palliative Care? Definition, Eligibility, and Role in Serious Illness Management
Palliative care is a medical therapy offering early and ongoing relief from symptoms and stress of any serious illness, whether treatable or not. By integrating with curative treatment, it enhances quality of life through pain management, psychosocial support, and care coordination. Patients can receive palliative care alongside chemotherapy, dialysis, or other life-prolonging interventions, ensuring comfort goals remain central throughout the disease course.
This inclusive model addresses needs from diagnosis through advanced stages, setting the stage for later hospice care if prognosis shortens. Next, we’ll compare eligibility windows and timing distinctions between these two approaches.
How Does Palliative Care Differ in Eligibility and Timing?
Palliative care can begin at diagnosis of a serious medical condition and continues regardless of prognosis or ongoing curative interventions. Eligibility encompasses any patient experiencing burdensome symptoms or emotional distress, from early-stage cancer to chronic organ failure. Early integration improves pain control, reduces anxiety, and often lowers hospital utilization over time.
By allowing concurrent therapy, palliative care sustains life-prolonging goals while enhancing daily well-being, bridging the gap until or beyond hospice enrollment.
What Are the Primary Goals and Services of Palliative Care?
Palliative care’s primary goals are symptom management, psychosocial support, and communication facilitation to align medical decisions with patient values. Services include pain and nausea control, counseling for depression or anxiety, nutritional guidance, and care-planning meetings. Family caregivers receive education and respite resources to reduce stress and improve at-home care.
This holistic framework promotes balance between disease-directed treatment and comfort-oriented interventions for sustained quality of life.
Which Serious Illnesses Commonly Receive Palliative Care?
Common palliative care populations include patients with metastatic cancer, congestive heart failure, chronic respiratory diseases like COPD, advanced kidney disease on dialysis, and neurodegenerative disorders such as ALS or dementia. Any condition with life-limiting potential and significant symptom burden qualifies.
Broad eligibility ensures palliative care’s supportive benefits reach those in early or mid-stage illness, promoting continuity and potentially easing transitions to hospice when appropriate.
What Are the Key Differences Between Hospice and Palliative Care?
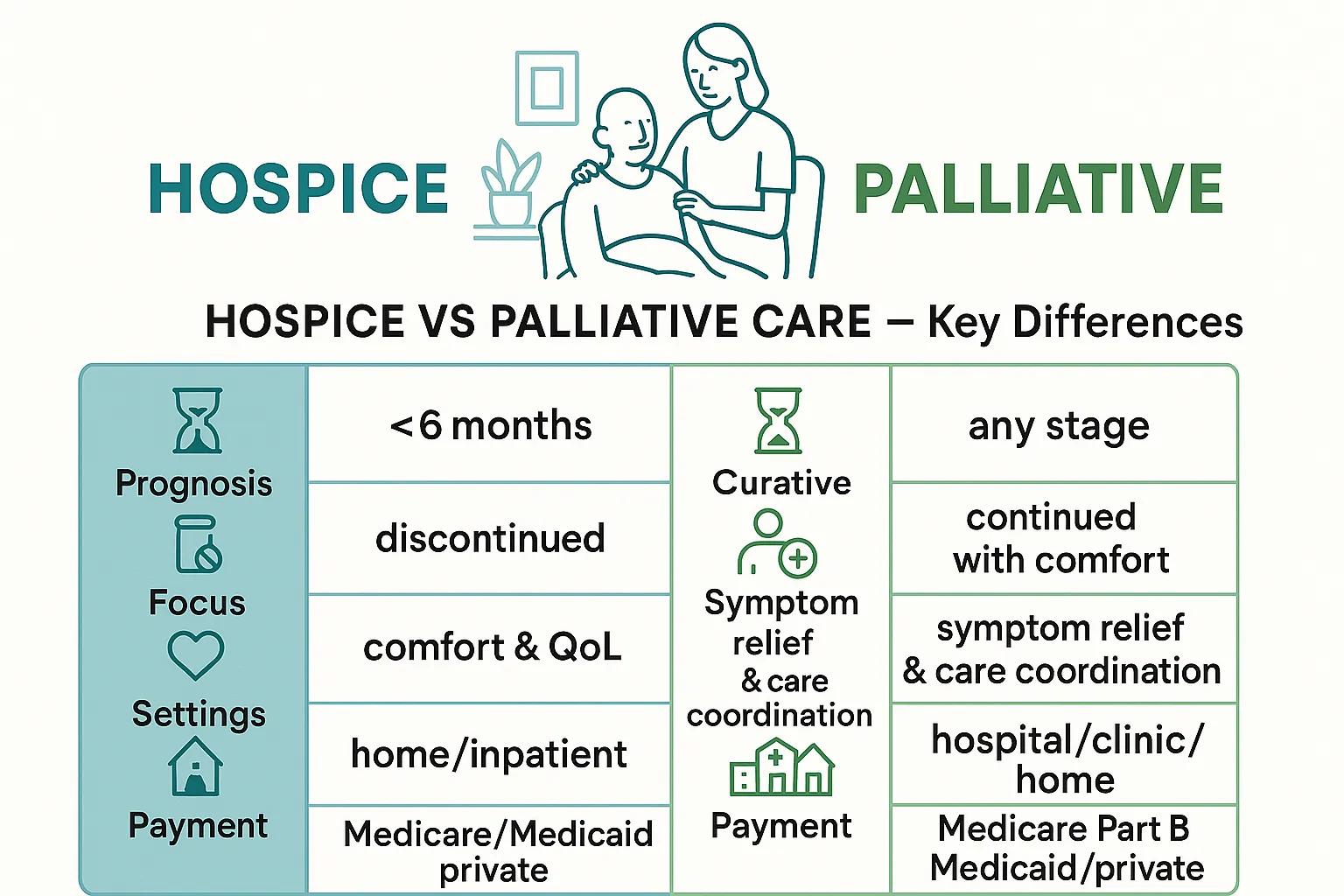
Comparing hospice and palliative care clarifies eligibility, treatment goals, and service delivery. The following table outlines core distinctions:
| Aspect | Hospice Care | Palliative Care |
|---|---|---|
| Prognosis Window | Less than six months | Any stage of serious illness |
| Curative Treatment | Discontinued | Continued alongside comfort measures |
| Focus | Comfort, quality of life, psychosocial support | Symptom management, communication, care coordination |
| Care Settings | Home, inpatient hospice unit, nursing facility | Hospital, outpatient clinic, home health, specialized center |
| Payment Coverage | Medicare hospice benefit, Medicaid hospice, private plans | Medicare Part B, Medicaid, private insurance covering consults |
How Do Eligibility Criteria Differ Between Hospice and Palliative Care?
Hospice eligibility hinges on a certified life expectancy of under six months and patient consent to comfort-only focus. In contrast, palliative care welcomes any patient with serious illness irrespective of prognosis or treatment goals. This distinction allows palliative interventions to start early, whereas hospice marks a later pivot to exclusively comfort-oriented support.
Recognizing these windows guides timely referrals and optimizes resource allocation.
How Do Treatment Goals and Approaches Contrast?
Hospice treatments aim solely at alleviating pain and distress without seeking disease reversal. Palliative care blends symptom relief with ongoing curative or disease-modifying therapies. For example, a patient may continue chemotherapy for tumor control while receiving palliative pain management, whereas hospice would discontinue chemotherapy in favor of comfort interventions.
Understanding these contrasts helps clinicians match care strategies to patient priorities.
What Are the Differences in Care Settings and Service Delivery?
Hospice services are delivered in patient homes, dedicated hospice units, or long-term care facilities by visiting interdisciplinary teams. Palliative care often begins in hospitals or outpatient clinics, then extends to home health or specialized centers based on patient need. Both models use physicians, nurses, social workers, and chaplains, but hospice personnel specialize in end-of-life coordination.
Care setting distinctions reflect each model’s timing and focus within the patient journey.
How Does Payment and Insurance Coverage Vary?
Hospice care is covered under the Medicare hospice benefit, which bundles room, board, medications for symptom relief, and equipment. Medicaid programs and many private insurers mirror this benefit. Palliative care consultations and services fall under Medicare Part B or equivalent commercial plan benefits, often billed per visit or service.
Knowing coverage nuances prevents unexpected expenses and informs financial planning.
When Should You Choose Hospice Care Versus Palliative Care? Patient Journey and Decision Making
Deciding between hospice and palliative care depends on prognosis, treatment goals, and patient values. Early symptom burden calls for palliative integration, whereas a clear terminal prognosis signals hospice referral. Aligning clinical indicators with personal priorities ensures tailored support, minimizing unnecessary interventions.
This decision-making framework bridges earlier definitions and sets the stage for exploring specific cues and preferences that guide timely transitions.
What Signs Indicate It’s Time to Consider Hospice Care?
How Can Palliative Care Be Integrated Early in Illness?

Palliative care can be introduced at diagnosis of any life-threatening condition by initiating consultations focused on symptom assessment and care planning. Embedding palliative specialists in oncology, cardiology, or neurology clinics ensures timely interventions for pain, fatigue, and emotional distress throughout treatment.
Early integration fosters continuous quality-of-life improvements and reduces crisis-driven hospital admissions.
Hospital-Based Palliative Care: Integrating Care with Cure
The impetus for Dame Cicely Saunders to initiate the palliative care movement likely stemmed from the necessity to counteract the impersonal, technocratic approach to death that had become prevalent in hospitals post-World War II. Palliative care is dedicated to alleviating the suffering of patients and their families. It extends beyond mere pain management to encompass the comprehensive management of any symptom impacting quality of life. Optimal care is achieved through early integration and thorough implementation across the entire disease trajectory. Proactive palliative care from the outset can contribute to improved clinical outcomes. At the end of life, it can enhance the potential for patients and families to experience a sense of growth, re
Hospital-based palliative care: A case for integrating care with cure, 2011
This early integration of palliative care emphasizes its role in improving outcomes and patient experience throughout the disease trajectory.
How Do Patient Preferences and Goals Influence Care Decisions?
Patient values—such as prioritizing independence, pain relief, or life extension—directly shape whether to pursue curative treatments alongside comfort measures or to transition fully into hospice care. Shared decision-making meetings help clarify goals, aligning medical options with individual priorities and cultural beliefs.
This values-driven approach ensures care pathways honor personal definitions of dignity and well-being.
Who Provides Hospice and Palliative Care? Roles of the Care Team and Support Services
Both care models rely on interdisciplinary teams to deliver holistic support. Physicians manage symptom protocols, nurses coordinate day-to-day care, and social workers facilitate psychosocial counseling and resource access. Collaboration with chaplains, therapists, and volunteers enriches spiritual and emotional well-being.
Understanding team composition reveals how each member’s expertise enhances patient-centered outcomes and prepares families for transitions.
What Is the Role of Physicians, Nurses, and Social Workers?
Physicians oversee medical management and prognostic discussions, while nurses implement care plans, administer medications, and monitor symptom relief. Social workers assist with advance care planning, connect families to community resources, and provide counseling to address emotional stressors.
These core roles integrate clinical and supportive elements, reinforcing comfort and autonomy.
How Do Caregivers and Family Members Participate in Care?
Family caregivers often administer medications, assist with activities of daily living, and notify professionals of symptom changes. Care teams provide training, respite options, and emotional support to reduce caregiver burden and enhance patient safety at home.
Active family involvement ensures continuity of care and shared responsibility for patient comfort.
What Additional Services Are Offered in Both Care Models?
Both hospice and palliative care offer bereavement counseling, volunteers for companionship, medical equipment loans (e.g., hospital beds, oxygen), and spiritual care by chaplains. Support groups and educational workshops help families navigate emotional and logistical challenges.
These services extend beyond direct medical therapy to address holistic needs and foster resilience.
How Are Hospice and Palliative Care Covered? Understanding Medicare, Medicaid, and Insurance Options
Financial planning for serious illness involves navigating benefits under government programs and private insurers. Hospice benefits package most end-of-life services under Medicare Part A, while palliative consultations fall under Part B. Medicaid and commercial plans generally parallel these structures, though coverage details vary by state and carrier.
Clarity on payment options prevents financial strain and ensures uninterrupted support.
What Does Medicare Cover for Hospice Care?
Medicare’s hospice benefit covers all services related to the terminal diagnosis, including nursing visits, medications for symptom relief, medical equipment, and spiritual counseling, with no additional copayments. Room and board in hospice facilities may incur daily coinsurance.
This comprehensive coverage simplifies billing and maximizes patient access to end-of-life support.
How Is Palliative Care Covered by Insurance and Government Programs?
Palliative care services are billed under outpatient or inpatient consult codes through Medicare Part B or equivalent private plan benefits. Typical coverage includes physician consultations, nursing visits, counseling sessions, and certain home health services, subject to deductibles and copays.
Understanding service-by-service billing helps anticipate out-of-pocket costs.
What Are the Typical Out-of-Pocket Costs and Financial Considerations?
Hospice care generally incurs minimal or no out-of-pocket expenses under Medicare benefits, though facility stays may require coinsurance. Palliative care costs depend on service frequency, provider type, and plan details, often involving copays for clinic visits or therapy sessions.
Early benefits verification and financial counseling reduce surprises and support budgeting efforts.
What Are Common Misconceptions About Hospice and Palliative Care? Clarifying Public Perceptions
Misunderstandings can delay referrals and limit access to beneficial services. Clarifying that palliative care works alongside curative treatments, hospice serves many illnesses beyond cancer, and choosing hospice does not equate to abandoning hope can reshape perceptions and encourage timely care transitions.
Addressing myths empowers patients and families to make informed decisions aligned with their values.
Can You Receive Curative Treatment While Getting Palliative Care?
Yes, palliative care can be delivered concurrently with disease-directed therapies such as chemotherapy or dialysis. Its symptom management and communication support enhance tolerance of aggressive treatments and reduce hospitalization risks.
This concurrent model distinguishes palliative care from hospice, which requires discontinuing curative interventions.
Is Hospice Only for Cancer Patients?
No, hospice eligibility extends to any terminal medical condition, including heart failure, COPD, dementia, and neurodegenerative disorders. Referral depends on prognosis and patient goals, not on a specific diagnosis.
Broad inclusion ensures timely comfort care across diverse end-of-life conditions.
Does Choosing Hospice Mean Giving Up Hope?
No, hospice focuses on realistic hope—comfort, quality time with loved ones, and dignity at life’s end—rather than cure. Many patients experience improved symptom control, reduced anxiety, and deeper emotional support through hospice’s holistic approach.
Reframing hope in terms of comfort and connection fosters meaningful experiences.
What Are Recent Trends and Statistics in Hospice and Palliative Care? Market Growth and Utilization Insights
The global palliative care and hospice market is projected to expand from $150 billion in 2025 to $260 billion by 2033 at a 7 percent CAGR. Aging populations and rising chronic disease prevalence drive demand. Yet only 14 percent of those in need currently receive palliative services, highlighting access gaps.
Technological adoption—especially telehealth and AI-driven symptom monitoring—is reshaping care delivery and personalization for home-based models.
How Is the Demand for Hospice and Palliative Care Changing?
Hospice utilization among Medicare decedents reached 51.7 percent in 2023, its highest rate since 2019. Palliative care consultations in hospitals have grown by over 20 percent annually, reflecting increased recognition of early symptom management benefits.
This rising demand underscores the need for workforce expansion and training to meet care needs.
What Are Current Utilization Rates and Access Challenges?
While hospice enrollment has become more common in high-income regions, rural and underserved areas face shortages of specialists and limited hospice facility availability. Palliative care access remains uneven, with only 50 percent of U.S. hospitals offering dedicated teams and even fewer home-based programs.
Addressing these disparities requires policy support and telehealth integration to extend reach.
How Are Technology and Home-Based Care Shaping Services?
Telehealth platforms now enable virtual symptom assessments, remote medication adjustments, and family conferencing, improving access in home-bound patients. AI-powered analytics predict symptom exacerbations, prompting proactive interventions that reduce emergency visits.
These innovations enhance continuity of care and patient empowerment outside traditional settings.
What Are Frequently Asked Questions About Hospice and Palliative Care?
What Is the Main Difference Between Hospice and Palliative Care?
Hospice care is exclusively for patients with a terminal prognosis under six months who forego curative treatments, focusing solely on comfort and quality of life. Palliative care serves any stage of serious illness, can continue alongside curative therapy, and centers on symptom relief and decision support.
Can You Have Palliative Care and Still Receive Curative Treatment?
Yes, palliative care integrates with curative or life-prolonging therapies to manage pain, nausea, and emotional distress without interrupting disease-directed interventions, enhancing overall treatment tolerance and patient well-being.
When Should You Choose Palliative Care Over Hospice?
Choose palliative care at diagnosis of a serious or life-limiting condition if you need early symptom management, emotional support, and care coordination while pursuing curative or disease-modifying treatments.
Who Pays for Hospice and Palliative Care?
Hospice care is covered under the Medicare hospice benefit, most Medicaid plans, and many private insurers with minimal out-of-pocket costs. Palliative care consultations are billed through Medicare Part B or equivalent commercial plan benefits, subject to copays and deductibles.
Hospice and palliative care each play vital roles in supporting patients through serious illnesses by prioritizing comfort, symptom relief, and patient-centered goals. Recognizing the eligibility windows, care team structures, and coverage options empowers timely referrals and informed decision-making. Whether integrating palliative services early or transitioning to hospice for end-of-life comfort, these approaches ensure compassionate, high-quality support aligned with the needs and values of patients and families.
